Why does it hurt to insert a tampon? It might be vulvodynia.
Inserting a tampon shouldn't make you cry, right? What about pleasuring yourself? (If you are crying, it shouldn't be because of pain). Then why does this happen?
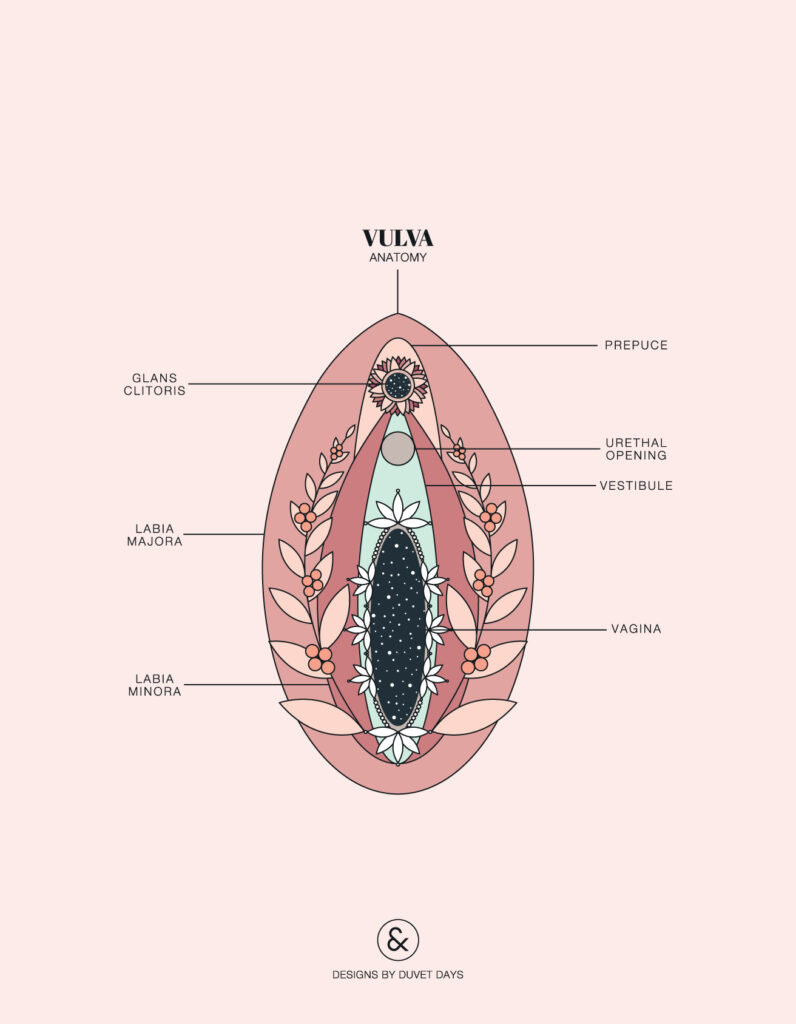
Vulvodynia (aka. vulvovestribular syndrome or vestibulodynia) is a chronic pain condition where there is vulvar inflammation in the vulvar vestibule area. Symptoms include: burning pain, redness and/or edema. About 20-30% of women will experience this condition in their lifetime.
This is a pretty complex condition, and I go into detail in the article below to give you all the background information you may possibly need. Before your eyes glaze over, I talk about who can help you with vulvodynia and what natural treatments look like towards the end of the article.
How is vulvodynia diagnosed?
Because we don't know why vulvodynia happens, it's considered a diagnosis of exclusion. This basically means that other conditions need to be ruled out before vulvodynia can be diagnosed. Also, you need to experience this pain for at least 3 months in order for it to be vulvodynia.
How is vulvodynia classified?
This is another condition that uses the primary/secondary classification.
Primary vulvodynia
Pain that is felt at first vaginal intercourse or tampon use.
Secondary vulvodynia
Pain that occurs after a period of pain-free sex.
What are the types of vulvodynia?
Provoked Vulvodynia (PVD)
This happens with sexual or non-sexual (ex. tampon insertion or contact with clothing) touch.
Localized
Burning pain is felt at the vestibule, by touch or penetration. You may also experience a sensation of tearing during sex.
Unprovoked Vulvodynia
Generalized
Aching or burning pain is felt around the entire vulva. Pain may radiate to perineum, thighs, bum, or the lower abdomen. Sitting, walking or tight clothing may make the pain worse.
Mixed
A combination of provoked and unprovoked pain.
Why does vulvodynia happen?
Bad news: we don't know why vulvodynia happens. But, we've got our theories!
Pain Theories
Believe it or not, there are 3 types of pain. Before you feel like you've been transported back to science class, let's briefly explain them:
-
Nociceptive pain: When pain is sensed at the vulvar vestibule (like when you're inserting a tampon), pain sensing nerve cells basically turn on, a signal is sent to the spinal cord which is then transmitted to the brain.
-
Inflammatory pain: This type begins with a nociceptive pain (ex. tampon touching the vestibule), but if it's prolonged then inflammation will occur. Inflammation is a release of inflammatory cells (cytokines, histamine, other cells you may have learned about in grade 10 bio). These cells will cause an increase in the blood vessels, leading to inflammatory cells seeping outside of the vessels (near muscles and fat) and causing swelling. The inflammatory cells can also turn on the pain cells around the site of the vestibule causing aching pain.
-
Pathological pain: Structural damage to the nervous system or abnormal function of the nervous system.
Anatomy
Tight muscles of the pelvic floor, may contribute to vulvodynia. Women with vulvodynia usually have tense pelvic floor muscles, they're unable to relax them and the muscles may not be all that flexible.
Any damages to the pudendal nerve (which innervates the vulva) may contribute to the pain, and might have happened during any surgeries (ex. C-sections) or prolonged child birth.
Common triggers
Last up, any vaginal (yeast or BV) or urinary tract infections, herpes simplex, trauma (using tools during delivery, including an episiotomy), back or hip injuries, hormonal changes (using birth control or simply perimenopause), past medications (like fungal cream) may cause vulvodynia.
Stress, anxiety, depression, pain-related fear, may also play a hand in this too.
Who can help treat vulvodynia?
Aside from your medical doctor, ob/gyn, or urogynecologist - there are other health professionals to consider adding to your team!
Pelvic Floor Physiotherapists
Remember how we talked about a tight pelvic floor? Before you attempt kegels (note: please don't do that), go see a pelvic floor physiotherapist first. They will be able to assess your muscle tone and provide you with the right exercises to do, to get the muscles functioning properly. Be forewarned that this often requires an internal exam using 1-2 fingers to get an idea of how your muscles are working.
Sex Therapists
It comes as no surprise that vulvodynia may put a damper on your sex life! Seeing a sex therapist may help with any negative thoughts or emotional distress associated with this condition. Because trauma like sexual abuse or divorce are likely to contribute to vulvodynia, these would likely be addressed as well.
Naturopathic Doctors
NDs, like me, take a look at the whole body to figure out what exactly is going on. Remember all those common triggers we mentioned? My goal is to figure out if any of those are in play, and if they are, I treat them. I might change up your diet, prescribe a few supplements, or do some acupuncture - but it's only because I want to feel better (because inserting a tampon shouldn't make you cry).
Acupuncturists
In the next section I'll talk about how acupuncture can be helpful when treating vulvodynia. But basically, an acupuncturist is able to look at your specific symptoms through a different lens to determine how it can be treated by Traditional Chinese Medicine. Prescribing herbs and doing acupuncture are their go-tos for treatment.
How is vulvodynia treated naturally?
This is a tough one. None of my texts, especially the ones about women's health mention vulvodynia. And, if you search Pubmed (the mecca of all scientific articles), very few appear. But that doesn't mean all hope is lost!
Vaginal Infections
If infections are the culprit, then I'll start my infections protocol. Basically, I'll make sure your immune system is keeping the bad bugs at bay, and you're vagina is full of good bacteria (don't worry, this doesn't involve yogurt tampons).
In on study looking at the vaginal microbiome, they found that the concentration of fungi was higher than the beneficial Lactobacillus! Therefore, making sure you have a healthy bacterial balance is key.
Stress
Although I might not be able to get rid of every single source of stress, I can help your body manage it better. Studies show that women with vulvodynia have a blunted cortisol response, meaning that your body may not be handing as stress as good as it can. Using particular vitamins and minerals, as well as herbs, we can work together to re-establish a healthy stress response.
Hormonal Changes
I've talked about the pill at length on the blog, but let's quickly talk about what it specifically does to vaginal tissue. When you take hormonal birth control, your estrogen levels (not the one provided by the pill) and total testosterone decreases. The pill can make the vulva more sensitive to muscle strain, increased pain, decreased lubrication, and increased dyspareunia. No bueno.
What does this mean for you? Well, we want to support hormone production, re-establish healthy hormone patterns, and help you to effectively detox the pill (we don't need fake estrogens hanging around in your body).
Acupuncture
Few studies have been done looking at the effectiveness of acupuncture and vulvodynia. If you've never had acupuncture done before (run, don't walk!), it has been shown to be an effective treatment for pain. It helps to balance the yin and yang within the body, as well as ensure that the vital energy, your Qi, is flowing without obstruction. Qi flows through the meridians of the body, where acupuncture needles are placed.
In a study from 2015, acupuncture was done in women with vulvodynia. Results showed that vulvar pain and dyspareunia were significantly reduced, although there was no significant change sexual desire, sexual arousal, lubrication, ability to orgasm or sexual satisfaction.
Final Notes
If you've made it to the end, thanks for sticking with me! As you can see, this is a pretty complex condition, and your healthcare team may need to be quite diverse. At the end of the day, our goal is to help you feel better.
If you found this information helpful, please sign up for my monthly newsletter called The Flow for great and informative content like this!
References
Thornton, A. and Drummond, C. (2015). Current concepts in vulvodynia with a focus on pathogenesis and pain mechanisms. Australasian Journal of Dermatology, 57(4), pp.253-263.
Pukall, C., Goldstein, A., Bergeron, S., Foster, D., Stein, A., Kellogg-Spadt, S. and Bachmann, G. (2016). Vulvodynia: Definition, Prevalence, Impact, and Pathophysiological Factors. The Journal of Sexual Medicine, 13(3), pp.291-304.
Vadala, M., Testa, C., Coda, L., Angioletti, S., Giuberti, R., Laurino, C. and Palmieri, B. (2018). Vulvovestibular Syndrome and Vaginal Microbiome: A Simple Evaluation. Journal of Clinical Medicine Research, 10(9), pp.688-692.
Schlaeger, J., Xu, N., Mejta, C., Park, C. and Wilkie, D. (2015). Acupuncture for the Treatment of Vulvodynia: A Randomized Wait-List Controlled Pilot Study. The Journal of Sexual Medicine, 12(4), pp.1019-1027.
